Blog Post
Beyond mammograms: What people with dense breasts should know about screening
Color
October is Breast Cancer Awareness Month, and this year, we are focused on an important, but often overlooked aspect of breast cancer screening: dense breast tissue and its impact on standard mammography. In this article, we’ll talk about what it means to have dense breasts, what alternative screening options might be recommended, the current state of insurance coverage of these alternative screening methods, and the role that both individuals and employers can play in promoting the right preventive behaviors.

When interpreting imaging results, clarity is everything. On a mammogram, breast tissue and fat appear dark, while tumors appear white – a contrast that can make cancer detection literally black and white. But 40% of people 40 years of age and older have dense breast tissue and 10% have extremely dense breast tissue. The challenge is that dense breast tissue also shows up as white on mammograms, just like a tumor. This can obscure the presence of cancer and make the picture of a person’s health far from clear.
Having dense breasts not only increases the challenge of detection but is also linked to a higher risk of developing breast cancer. Understanding breast density, how it impacts screening, and what people can do about it is critical for early detection and in some cases, effective treatment.
For years, people were not always made aware of whether they had dense breast tissue or what dense breasts meant in terms of cancer detection. Recent FDA regulations now require mammogram providers to inform people if they have dense breast tissue and document breast density on the report. This is an important step for people across the US to better understand their breast cancer risks and to take action to maintain their health. The new regulation also makes it more important than ever to be proactive about screening.
What does it mean to have dense breasts?
Having dense breasts just means that there is more fibrous or glandular tissue and less fatty tissue. On a mammogram, dense tissue appears white—just like cancer—making it difficult to differentiate between the two. You are more likely to have dense breast tissue if you are younger, pregnant or breastfeeding, are taking hormone replacement therapy (HRT), or have a lower body weight.
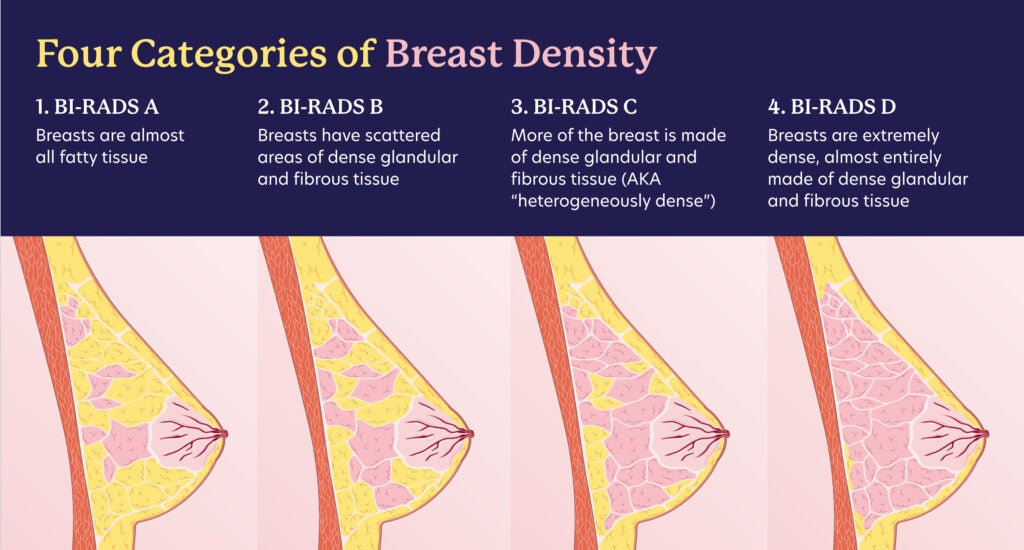
Breast density is classified into four categories according to the Breast Imaging Reporting and Data System (BI-RADS) from the American College of Radiology:
- BI-RADS 1 (Almost Entirely Fatty): The breasts are almost entirely made up of fatty tissue. Detection of cancer is easiest in this category, which accounts for about 10% of people.
- BI-RADS 2 (Scattered Areas of Fibroglandular Density): Some areas of dense tissue are present, but the majority of the breast is fatty. Cancer detection is still relatively straightforward for the 40% of people in this category.
- BI-RADS 3 (Heterogeneously Dense): Many areas of the breast are dense for 40% of people, which can obscure small masses and make cancer harder to detect.
- BI-RADS 4 (Extremely Dense): In 10% of people, breasts are extremely dense, significantly increasing the difficulty in detecting abnormalities on a mammogram.
While breast density often decreases with age, certain genetic or lifestyle factors can contribute, such as alcohol consumption.
What is the impact on cancer detection?
As dense breast tissue and cancer both appear white on a standard mammogram, mammography is less sensitive in people with dense breasts and can lead to cancers going undetected. Conversely, people with dense breasts may be called back unnecessarily for stressful follow-up testing as radiologists work to interpret these hard-to-read images.
Because dense breast tissue itself is associated with a higher risk of developing breast cancer, knowing your breast density is important.
As of March 2023, the FDA requires mammogram providers to notify people if they have dense breast tissue. Mammogram reports must now clearly state a person’s breast density category and offer recommendations for follow-up. This regulation is part of an effort to improve awareness and empower people to take control of their breast health.
Knowing your breast density category is critical for understanding the accuracy of your mammogram – and your alternative screening options. It’s important to note that insurance coverage for these supplemental screenings varies. Some states have laws around insurance coverage of follow-up screenings for people with dense breasts, but this is not uniform across the country. As a result, a person may need to review their insurance policy or consult with their healthcare providers to understand if they will face out-of-pocket costs for these additional screenings. With this new regulation, it’s important to be able to advocate for the right screenings based on breast density, and for employers and health plans to consider updating their coverage options to support necessary follow-up tests.
What are additional screening options?
Because standard mammograms may miss cancers for people with dense breasts, additional tests may be recommended, including:
- Ultrasound:
- Whole-breast ultrasound can be used alongside mammograms to provide a clearer image of dense tissue.
- The technology uses sound waves to produce images, helping detect small tumors that mammograms may miss.
- MRI (Magnetic Resonance Imaging):
- Breast MRI uses magnetic fields and radio waves to create detailed images of the breast.
- It’s often recommended for people with a high risk of breast cancer, including those with dense breasts.
- MRI is more sensitive than mammography, but it’s also more expensive and not typically used for routine screening in average-risk people.
- Tomosynthesis (3D Mammography):
- Tomosynthesis takes multiple images of the breast from different angles, creating a 3D image.
- This method can provide more detailed images than a standard (2D) mammogram and can be particularly useful for people with dense breasts.
- Contrast Enhanced Mammograms:
- Contrast-enhanced mammography (CEM) involves injection of iodinated contrast materials to help make the difference between a potential tumor and dense breast tissue more clear.
- While new, CEM has been found to help improve accuracy compared with digital mammography.
- The method does slightly increase a person’s radiation dose and carries a small risk of adverse reactions to contrast materials.
How to advocate for your health
Ask about your breast density
- After receiving a mammogram report, ask your healthcare provider if you have dense breasts and what that means for your screening.
- Understanding your breast density helps you make more informed decisions about whether additional screening is needed.
Discuss screening options
- If you have dense breasts, talk to your doctor about whether you might benefit from supplemental screening such as a breast ultrasound or MRI.
- Don’t hesitate to ask for more information about breast density and how it impacts your cancer risk.
Know your personal risk factors
- In addition to breast density, consider other risk factors like family history, genetic predispositions, and lifestyle factors.
- Consider genetic screening. Certain genetic factors, such as the BRCA1 and BRCA2 genetic mutations put a person at increased risk of several types of cancer, including breast.
- If you are at increased risk, your doctor may recommend more frequent screenings or a different combination of tests.
How to advocate for your employees and members
Offer support through comprehensive benefits
- Understanding the scope and implications of breast density, employers should ensure their health benefits include supplemental screening options, such as ultrasound or MRI.
- Offering flexible, comprehensive coverage allows people to access the screening tools that best suit their individual needs.
Address breast cancer health proactively
- Employers and health plans can play a crucial role in supporting their employees by making sure that benefits cover advanced imaging technologies that improve early detection in dense breasts.
Breast density can make traditional mammography less clear. That is why it is important that all of us – individuals, employers, and health plans – have a critical role to play in understanding the risks associated with breast density and the prevention and detection of breast cancer.