News & Articles
Prostate cancer is one of the most important health issues for men
Lauren Ryan

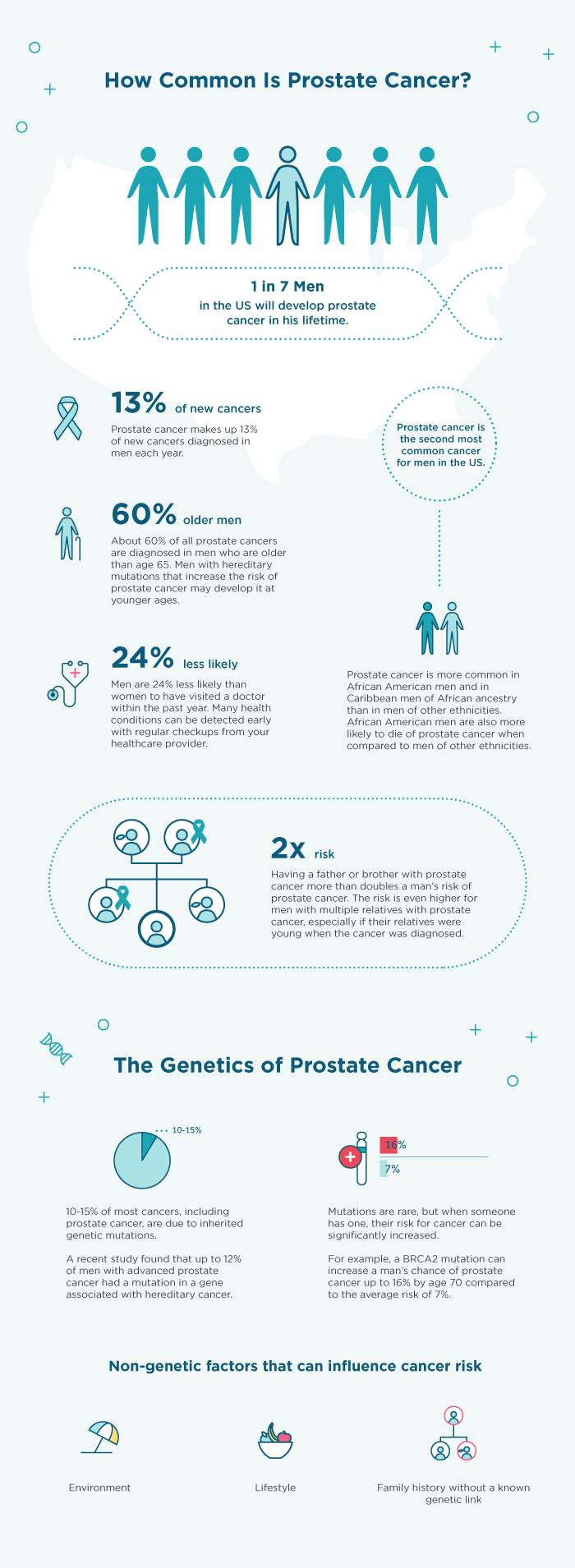
About 1 in every 7 men in the US will develop prostate cancer in his lifetime. While most prostate cancers grow slowly, some can grow and spread quickly. There are a number of things you can do to be proactive about your risk.
What can you do?
- Talk to your healthcare provider at your next visit about prostate cancer screening recommendations based on your age and risk factors.
- Some options for prostate cancer screening include a blood test called PSA and a digital rectal exam (DRE).
- The age to start and the frequency of screening may vary.
- Your doctor may recommend screening less often or not at all after a certain age, and only if you are very healthy with little or no other health concerns.
What else should you consider?
Certain factors can increase risk above average. For example:
- Ethnicity: Men of African American or Caribbean American ancestry are more likely to develop prostate cancer compared with Caucasian men.
- Family history: Relatives of men with prostate cancer may have a higher risk, even without a known genetic link.
- Genetics: Inherited mutations in certain genes may increase risk to develop prostate cancer. Some men may want to consider genetic testing for these mutations, as a recent study shows they may increase risk, especially for advanced prostate cancer.¹
It’s important to include all of this information in a discussion with your healthcare provider to make sure you are receiving tailored screening guidelines based on your risk.
Did you know men are much less likely than women to visit a doctor, even though a discussion with a healthcare provider can be life-saving? Talk to your provider about prostate cancer screening and encourage all of the men you care about to start a conversation with their provider during the month of November. Learn more at color.com.
- Pritchard CC, Mateo J, Walsh MF, et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N Engl J Med. 2016;375(5):443–53.



