More than meets the eye: breaking down the $43 billion price tag on cancer screening
More than meets the eye: breaking down the $43 billion price tag on cancer screening
At first glance, $43 billion seems like an enormous sum. However, when we break down these costs, we find that a significant portion is attributable to facility fees, lab charges, and administrative expenses rather than the screening procedures themselves. Facility charges, for instance, are the largest contributor to colonoscopy costs.
It is also important to view the $43 billion figure in the broader context of cancer-related healthcare costs. The same study cites estimates that the annual cost to the U.S. healthcare system for cancer screening, treatment, and survivorship likely exceeds $250 billion. In this context, screening costs represent a relatively small proportion of total cancer-related expenditures, especially considering their potential to significantly reduce more expensive late-stage treatments.
The value of cancer screening extends far beyond its immediate costs. Early detection often leads to less aggressive and less costly treatments.
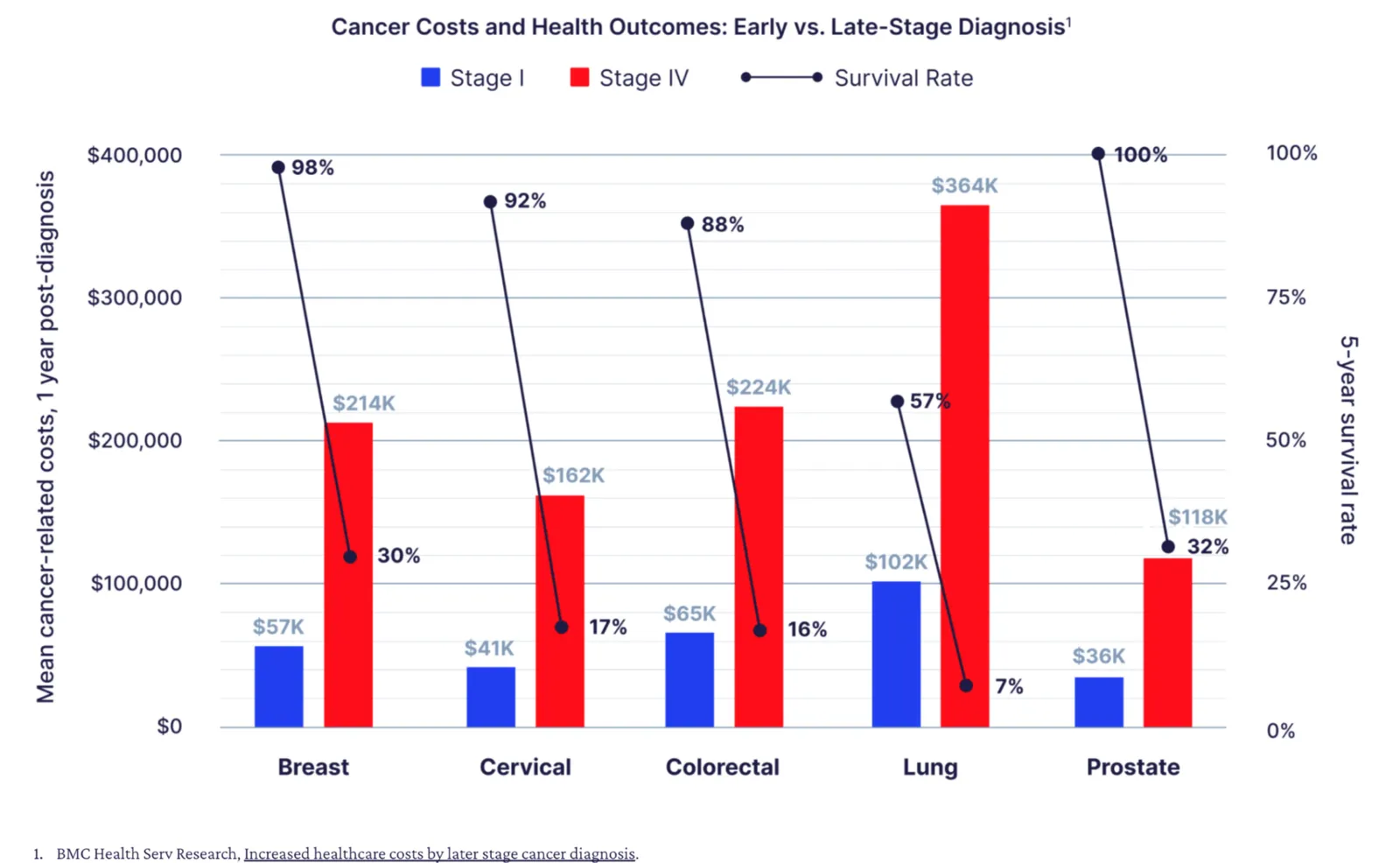
The study itself acknowledges that earlier-stage diagnosis is associated with decreased treatment costs and improved quality of life. Some screenings, like those for colorectal and cervical cancer, can even prevent invasive cancers by detecting and removing precancerous lesions. These prevention and early intervention aspects have significant long-term economic benefits that may not be fully captured in the $43 billion figure.
It’s also worth noting that cancer screening has been a contributing factor to decreasing cancer mortality rates. The study reports that cancer death rates decreased by 2.1% per year from 2015 to 2019, with notable decreases in cancers for which screening is recommended. While screening isn’t the sole factor in this reduction, its role cannot be overlooked.
Rather than questioning the fundamental value of screening, we should focus on optimizing these programs to maximize their cost-effectiveness. This could involve more effectively targeting high-risk populations, improving the efficiency of screening delivery, reducing unnecessary follow-up procedures, and implementing more cost-effective screening technologies.
A comprehensive economic analysis of cancer screening should also consider broader societal benefits, such as improved quality of life for patients diagnosed early. These factors, while not captured in the $43 billion figure, contribute significantly to the overall value of screening programs.
While the annual cost of cancer screening in the United States is substantial, it represents an investment in public health that yields considerable returns in terms of lives saved, improved quality of life, and long-term cost savings in cancer treatment. As we continue to refine and improve our approach to cancer screening, the focus should be on optimizing these programs rather than questioning their fundamental value. When viewed holistically, the economics of cancer screening paint a picture of a vital and cost-effective component of our healthcare system.